Translational Pulmonary
& Immunology Research Center
& Immunology Research Center
TPIRC leverages the power of big data analytics, traditionally used in commercial settings, to drive medical research and treatment advancements. This innovative approach translates vast amounts of data into actionable insights, shaping personalized treatment plans and improving patient outcomes.

At the Translational Pulmonary and Immunology Research Center (TPIRC), research is at the heart of the discoveries that allow us to develop individualized treatment for each one of our patients.
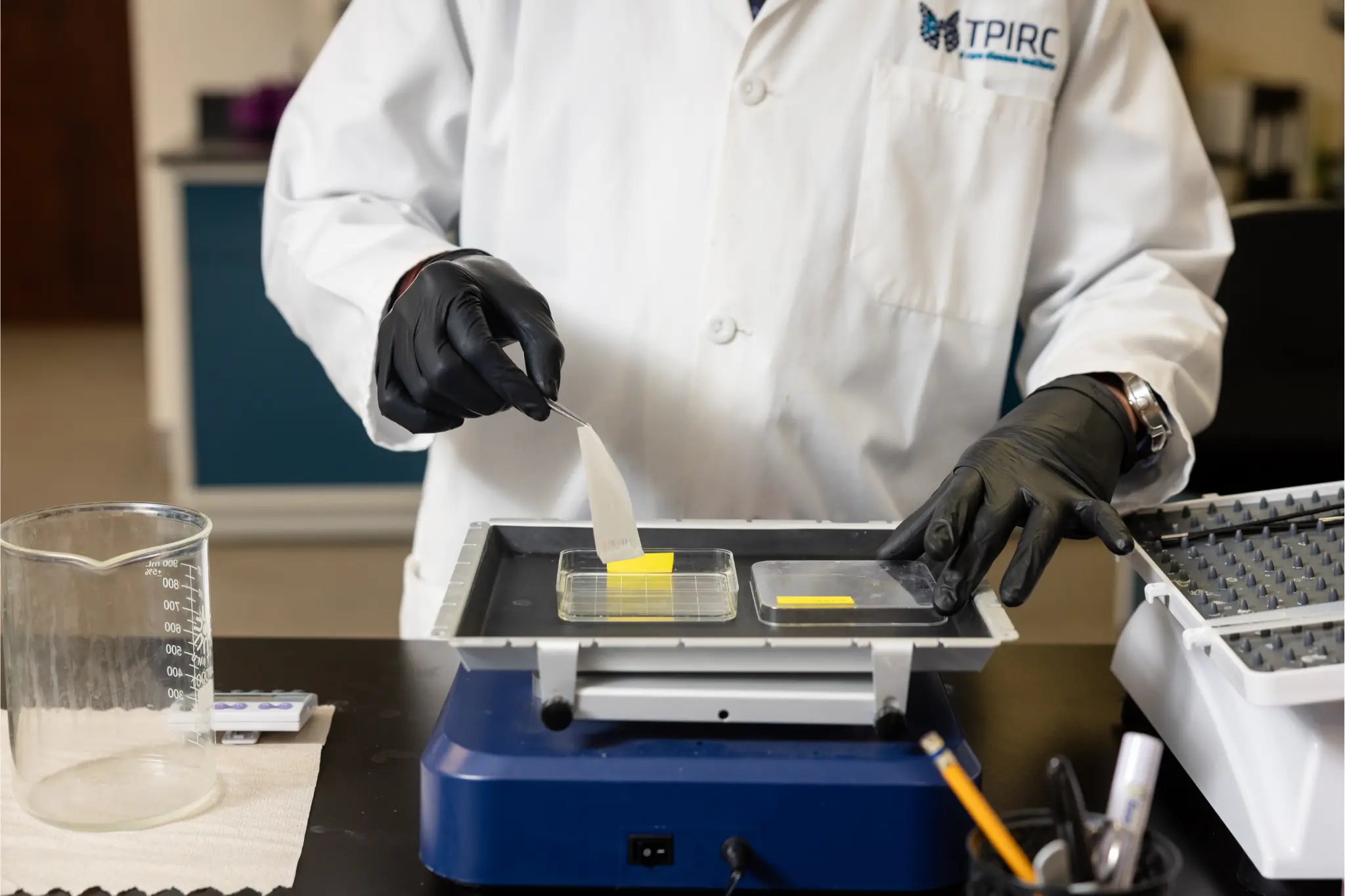
Our facilities are equipped with cutting-edge technology set up for a proteomics and cell and molecular biology core in pursuit of protein characterization and biomarker discovery. Each patient contributes millions of additional data points that continue to reveal and reinforce patterns that lead to advancements in care and breakthrough discoveries. Over time, our already successful, integrated approach can be even further refined with the TPIRC Biobank for more and more precise food allergy treatment.

Nathan Marsteller is a scientist with over fifteen years of experience in the biological sciences, specializing in immunology, pulmonology, and molecular biology. He holds a Ph.D in Biological Sciences from the University of Nebraska-Lincoln.
As the Director of Research at the Translational Pulmonary and Immunology Research Center (TPIRC (pronounced tea-perk)) in Long Beach CA since 2017, Dr. Marsteller has builtd a research laboratory with a focus on translational science that improves the lives of patients at the Food Allergy Institute and Millers Children’s Hospital by leveraging massive amounts of data to optimize various research projects, innovative diagnostic approaches, patient-focused methodologies, and the study of interactions between the immune system and genetic regulation in rare diseases, particularly in the realm of allergy and lung development.
In addition to his role at TPIRC, Dr. Marsteller serves as Research Faculty at the Pediatric Pulmonology Division of Miller Children’s Hospital, University of California Irvine. In this capacity, he plays a crucial role as the Primary Research Mentor for fellows in the Pulmonology Fellowship program. His commitment to guiding the next generation of researchers and physicians is evident in his leadership and dedication to fostering their growth.
His commitment to advancing scientific discovery in the food allergy space is reflected in his role as the Principal Investigator for the TPIRC Biospecimen and Data Resource (The TPIRC Biobank) since 2020. This initiative stores and manages biological samples and associated patient data, contributing significantly to the advancement of medical science and the discovery of new treatments and diagnostics for patients suffering from food anaphylaxis.
His innovative approach helps drive discovery and optimize patient therapeutics through basic science, translational science, and mentorship.
Anh Duong is a Research Laboratory Manager at TPRIC with over 30 years of experience in bio-immunological research. In her current role, she plays a key part in the design and execution of various scientific projects, including BPD, cystic fibrosis neutrophils, and mustard protein extraction. Her responsibilities also include validating immunological assays for analyzing human serum cytokines, training and mentoring fellows, college students, and volunteers, as well as developing protocols and laboratory operating procedures. Additionally, she oversees the maintenance of scientific equipment, laboratory disposables, chemical inventory, and safety records.
Anh graduated with a Bachelor of Science in Clinical Dietetics from the University of Pittsburgh in Pennsylvania and later earned an MBA from the University of Phoenix. She was quickly drawn to biological research early in her career. She gained extensive in-vivo and in-vitro experience across various industries, starting at the National Institutes of Health (NIH), where she was trained in identifying novel human brain proteins.
She then joined a start-up company, where she played a key role in setting up a Class 10,000 clean room for research focused on curing Type II diabetes through the implantation of encapsulated porcine islets of Langerhans. Over the next 20 years, Anh worked with various medical device and biopharmaceutical companies, including leading efforts on the dry eye murine model for ocular inflammation and contributing to the development of Restasis eye drops. Her exceptional work earned her the prestigious “Hidden Gem Award,” the highest honor given to a single employee, accompanied by a monetary prize.

Dr. Tripathi has expertise in Pulmonary immunology, infectious disease, Host-pathogen interaction, and drug discovery. Dr. Tripathi has a critical role in the research being conducted at the Center. Dr. Tripathi, in collaboration between TPIRC and Hastings Center for Pulmonary Research, Keck School of Medicine, University of Southern California (USC), is studying bronchopulmonary dysplasia and noninvasive ventilation strategies (continuous positive airway pressure therapy, CPAP) and their effects on lung development at the structural, cellular, molecular, and genetic level. He has outstanding skills in developing analytical methodologies for food allergens characterization, and allergen-specific host immune response especially focused on T cell functions for individual patients. Before joining TPIRC as a Research Scientist, Dr. Tripathi was a research fellow at the UND School of Medicine and Health Sciences and has explored the molecular signaling of host-pathogen interaction, with special attention to bacterial and viral pneumonia (pneumosepsis). He has extensive work experience with transgenic mouse strains as preclinical disease models. Dr. Tripathi did his doctoral research work at CSIR- Central Drug Research Institute and obtained his Ph.D. degree from Jawaharlal Nehru University, which is a top-ranked university in India, where his work was focused on “designing, understanding the structure-function relationship, and the development of antimicrobial peptide-based novel antibiotics.”
Several security measures are put in place for our HIPAA-compliant biobank including passwords, varying levels of access, and use of firewalls and encryption. As part of our security measures, identifiers will be removed from samples and research files and replaced with a code to ensure privacy.
We hope you will join the biobank so that we can better understand this disease and help future generations of kids achieve food freedom! For more information contact biobank@tpirc.org
With the Biobank, we can use the serum samples from our participants to identify and characterize appropriate allergens through several techniques including immunologic, biochemical, and structural characterization.
We can identify the IgE reactivity profile of allergens by immunoblotting and determine the clinical relevance of specific allergens with ELISA. We may also be able to identify cross reactivities with ELISA inhibition.
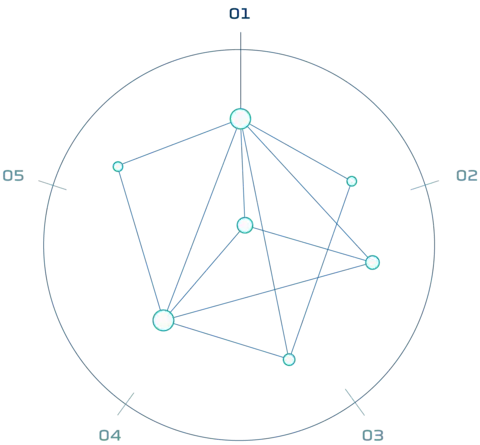
Precision medicine advances science and medical treatment in a complex yet effective approach of the “n=1”. The n of any study is the number of subjects. With more than 8,000 patients treated for severe food allergic disease, the N of our Institute exceeds that of many worldwide. TPIRC focuses on the development of cutting edge, individualized treatment protocols for orphan diseases utilizing comprehensive diagnostic tools, and patient-driven research.
Translational research is a “bench to bedside” approach. The goal of which is to improve patient outcomes. Each patient has hundreds of biomarkers analyzed prior to treatment. These data give us insight into the unique immune profile of each patient. We utilize this data to characterize, analyze, and improve patient treatment modalities. During this analysis we have the potential to discover novel biomarkers that can help us better understand the complexities of hard to treat patients with rare and orphan diseases. This approach aids in creating the best diagnostics possible. Additionally, the long-term follow-up of patients involving the standardization of biomarkers will be critical to the lifelong treatment outcomes of food allergy patients.
Research to characterize disease states at the DNA, RNA, protein, and immune cell levels is critical to the development of newer treatments for food allergy as well as various pulmonary diseases. Identification of novel biomarkers that can predict and reflect short-term molecular changes and long-term impact changes toward immune system tolerance is key. Such markers are currently not available but with the participation of the Tolerance Induction Program (TIP) patients in the TPIRC Biobank, the discovery of such markers is possible and patients undergoing TIP can receive the best molecular and clinical outcomes possible.
Food anaphylaxis diagnostic marker compilation in machine learning design and validation
Randhawa, I.,Groshenkov, K., Sigalov G.
Demographic, Clinical and Diagnostic Correlation of Almond Allergy in a Cohort of Nut Allergy Patients.
Marsteller, N.L., Morphew, T., Randhawa, I., Ann. Allergy (2020).
Evaluating the potential allergenicity of dietary proteins using model strong to non-allergenic proteins in germ-free mice….
Marsteller, N.L. et al. Food Chem Toxicol, 111398 (2020).
Cystic fibrosis patients at risk for disease progression marked by decline in FEV1% predicted: development of the cystic fibrosis risk of di…
Marsteller, N.L., Nussbaum, E., Morphew, T. & Randhawa, I.S. J Thorac Dis 11, 5557-5565 (2019).
Tolerance Induction Program Effect Explains Variation in Wheal Size, sIgE, and IgG4 in Peanut Allergic Children….
Randhawa, I., Marsteller, N.L., Morphew, T. J Allergy Ther 10:2 (2019)
Allergy Evaluation During Hospitalized Asthma Improves Disease Management Outcomes.
Brock, J.P., Nussbaum, E., Morphew, T.L., Marsteller, N.L. et al. SN Comprehensive Clinical Medicine. 1, 328-333 (2019).
Correlation of negative skin-prick test results for tree nuts and successful tree nut challenges among children with peanut allergy….
Randhawa, I., Morphew, T. & Marsteller, N.L. Allergy and asthma proceedings : The Official Journal of Regional and State Allergy Societies. 39, 456-460 (2018).
Experimental evaluation of the importance of colonization history in early-life gut microbiota assembly….
Martinez, I., & Marsteller, N.L et al. Elife 7 (2018).
TPIRC quantifies neutrophil infiltration in CF lungs and evaluates its contribution to disease progression.
TPIRC employs a model system to analyze the impact of non-invasive ventilation strategies at the structural cellular and molecular levels.
TPIRC investigates the influence of anxiety on treatment outcomes in children undergoing biosimilar protein immunotherapy for food allergies as well as the influence of food allergies on the mental health of parents and patients.
TPIRC investigates the susceptibility of food-allergic children to SARS-CoV-2 infection. We have found that there is no solution.
TPIRC expands the repertoire of allergens for biosimilar protein immunotherapy by characterizing lesser-studied food allergens and binding characteristics of their components with participant serum from the TPIRC Biobank.
TPIRC analyzes the impact of cesarean delivery on gut microbiome composition in newborns and its potential association with food allergy development.
TPIRC investigates the prevalence of almond allergy among a group of nut allergy patients to determine evaluate the correlation of almond allergy specific to demographic, clinical, and diagnostic markers prior to initiating OIT.
TPIRC investigates the prevalence of walnut allergy among a group of nut allergy patients to determine evaluate the correlation of almond allergy specific to demographic, clinical, and diagnostic markers prior to initiating OIT.
TPIRC explores CPAP as a protective measure against lung damage in premature infants with BPD. Combining CPAP with mild hyperoxia in mice normalized tissue damage and increased gene markers for repair, suggesting CPAP’s potential to mitigate BPD development.